Ohio State wide receiver Johnnie Dixon missed his freshman season and became eligible for a medical redshirt after having surgery on both his knees this past fall. The four-star recruit out of Palm Beach Gardens, Fla., was reportedly treated for tendinitis, which he has dealt with since at least his junior year of high school.
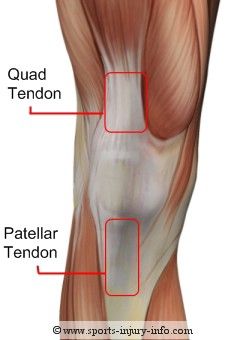
Tendons are like cords. They connect muscles to bones. The patellar tendon is found near the front of the knee. It’s an extension of the tendon of the quad muscles. It runs from the bottom of the kneecap (patella) to connect down to the shinbone (tibia).
Tendinitis is actually a misnomer. Diseased tendons have an umbrella diagnosis of “tendinopathy,” and when used in reference to the knee, this most often refers to patellar tendinosis.
The suffix “-itis” suggests inflammation as the cause of this condition. Rather, the diseased tendon has areas of degeneration due to chronic microtrauma (little tears which accumulate over time and lead to deterioration of the tendon tissue). The suffix “-osis” more accurately reflects this chronic degenerative pathology. It’s simply a wearing out of the over-stressed tendon.
Why does the tendon become worn out? This can be attributed to its relationship with the quad muscles. The patellar tendon is aggravated by excessive jumping activities. In fact, patellar tendinopathy was once referred to as “jumper’s knee.” The tendon is also provoked by quick directional changes, which could explain the condition in a wide receiver.
Tendinosis leads to pain and decreased function, and when this condition does not respond to conservative treatment (rest, activity modification, strengthening), surgery sometimes becomes the next viable alternative.
There are a few surgical options when addressing diseased patellar tendons. Open patellar tenotomy is one commonly used method. “Open” refers to the surgical approach; the knee is dissected open for easy access to the tendon. Tenotomy refers to making a surgical cut in the tendon.
In this procedure, the surgeon makes a cut or multiple cuts in the tendon to alert the body to recruit healing factors to the area. Why would a surgeon make cuts in the tendon when microtears created the issue in the first place? It seems counter-intuitive, right?
This operation works because a large surgical incision is different from the tiny pathological tears. Performing a tenotomy is kind of like waking the tendon back up. When tissue is chronically sick, the body can eventually give up the acute healing process. It’s as if the body just decides to accept the diseased tendon. This isn’t really fair, because the symptoms are still present, but the recovery is halted. The tenotomy is used to draw attention to the injury again. It kick-starts an organized recovery process.
Sometimes the surgeon also performs a debridement, which is a clean up procedure. Sick, degenerated tissue is scraped off the tendon to get it out of the body and make room for the healthy tissue to thrive.
The idea of a tenotomy and debridement is similar to aerating your lawn. You perforate the soil to allow air, water, and nutrients to flow freely. This creates a better environment for grass to grow and fill in dead patches. The grass of your patellar tendon is healthy tissue that fills in the patches the diseased tissue once occupied.

After successful patellar tendon surgery, it takes between 6 and 12 months for an athlete to return to full competition. Because of this relatively long recovery time, surgery is only recommended after the conservative treatment options have been exhausted. Since Dixon had been dealing with pain in both of his knees for 2-3 years before his operation, we’re happy he invested in this treatment, and we’re excited to see the kind of talent he can bring to Ohio Stadium when he’s ready.
References:
- Brukner, Peter and Khan, Karim. Clinical sports medicine. McGraw Hill, 2006.
- Peers, Koen HE, and Roeland JJ Lysens. "Patellar tendinopathy in athletes." Sports Medicine 35.1 (2005): 71-87.
- Testa, V., et al. "Ultrasound-guided percutaneous longitudinal tenotomy for the management of patellar tendinopathy." Medicine and science in sports and exercise 31.11 (1999): 1509-1515.


